Ventricular Tachycardia
Monomorphic ventricular Tachycardia
- Usually 120-300 beats/min
- Rhythm regular or almost regular
- ↑ QRS duration > 0.12 sec
- V1: often RBBB morphology
- Fusion or capture beats
- Bizarre QRS complex and axis (axis negative in 1 and aVF), but may have a BBB morphology
- Evidence of AV dissociation ( Cannon "a" waves in the JVP, P waves, capture beats, fusion beats, concordance in the chest leads )
- VA block with Wenckebach
- Concordance V1 to V6 (also seen with WPW)
- If LBBB pattern likely to be coming from right ventricle (RBBB pattern likely from left ventricle)
RVOT
- Monomorphic VT
- Exercise induced
- LBBB morphology with inferior axis (DDx ARVD)
- Adenosine sensitive (cAMP mediated)
- Good prognosis
- Treat with β-blockers before radio ablation
Differential diagnosis
- Could this be SVT with aberrant conduction or a pre-existing bundle branch block? link
- In unstable patients: See Resusc Council UK algorithm(Hover for Algorithm)
- In stable patients:
- Treat ischaemia, correct electrolytes. Consider immediate cardioversion
- Choice of drugs in stable patients: Amiodarone, Lidocaine, procainamide, sotalol
- Avoid procainamide and sotalol if clinical signs of impaired LV fxn
- Choose one agent only, and seek expert advice if you are at all unsure
Polymorphic ventricular tachycardia
- Irregular broad complex tachycardia
- Variable QRS morphology
- Often has an underlying cause such as electrolyte disturbance, toxins, or ischaemia
- Leads to haemodynamic collapse
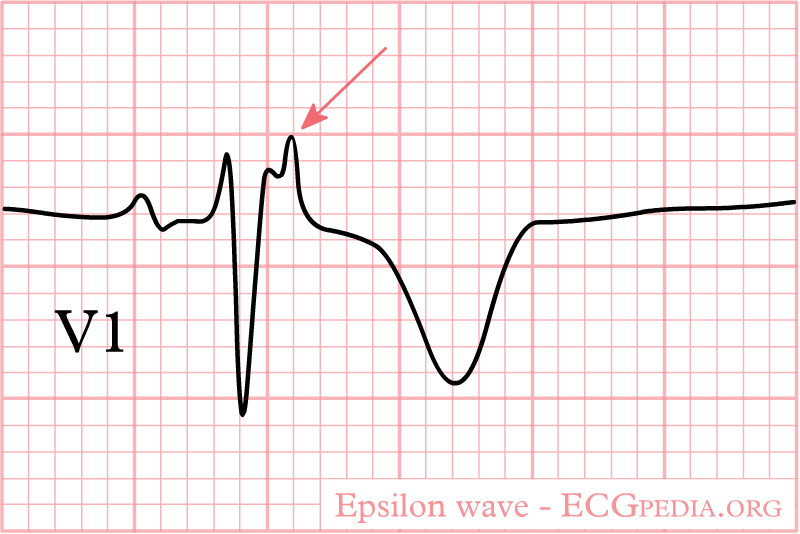
Arrhythmogenic Rt Vent Dysplasia (ARVD)
- Fibrous tissue in Rt Vent particularly young patients
- LBBB morphology during VT
- ECG features:
- Epsilon waves
- T wave inversion V2-V3
- Incomplete RBBB (particularly V1-V3)
- Paroxysmal VT with LBBB pattern
- DDx RVOT (above)
- Involve cardiology:
- 1% die per year
- Hereditary (screen 1° relatives)
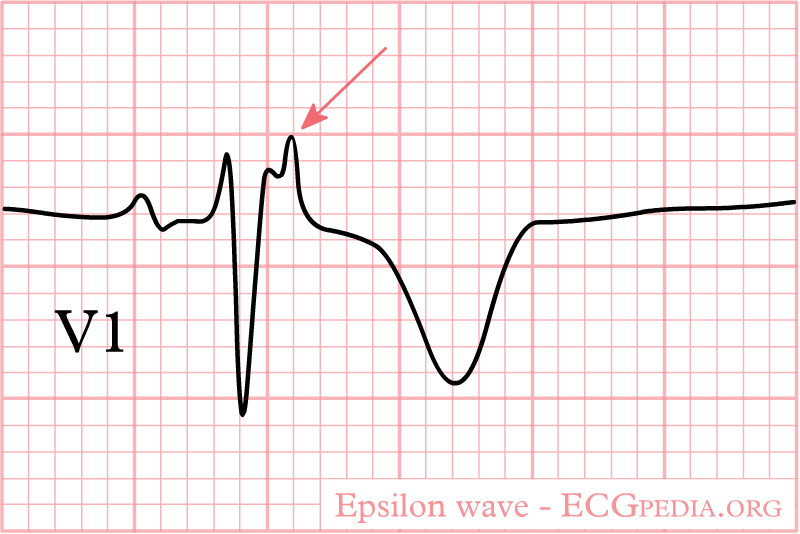 Image from ECGpedia.org
Image from ECGpedia.org
Management
- In unstable patients: Go to the broad complex tachycardia treatment Resusc Council UK algorithm
- In stable patients:
- Treat ischaemia, correct electrolytes. Consider immediate cardioversion
- Choice of drugs in stable patients: Amiodarone, Lidocaine, procainamide, sotalol, β-blockers
- Avoid procainamide & sotalol if clinical signs are suggestive of impaired LV fxn
- Lidocaine or β-blockers may be indicated if you suspect acute ischaemia
- Choose one agent only, and seek expert advice if you are at all unsure
Last review Dr Íomhar O' Sullivan 17/01/23.